A 65 year old male patient with complaints of fever and sob
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment.
Complaints:-
Patient was brought to casualty with complaints of fever since one week
breathlessness since one day
history of presenting illness:-
Patient was apparently symptomatic one week back then he developed cough and cold which was insidious in onset associated with sputum, which was greenish in color and mucoid in nature,no aggravating factors no relieving factors then he developed the fever which was insidious onset , gradually progressive, it is of high grade, associated with chills and rigors for which he took medication from an RMP which got subsided but reappeared two days back
Patient complains of increased frequency of urine passage during night Times since 7 days( 4 to 5 times)
Complaints of decreased appetite since 4 days
Complaints of nausea since 4 days
Patient feels dehydrated Since 4 days complaints of dryness of lips
Complaints of shortness of breath since four days which was initially grade 2 which now progressed to grade 4 since last night.
Past history:-
No history of similar complaints in the past
complaints of pain in bilateral knee joints since 5 years for which he was using NSAID's
Not a known case of hypertension,TB, epilepsy,cva,CAD
Had a history of right tbl fracture 5 years back
Personal history:-
Patient takes normal diet, but due to decrease appetite he started to eat in less amount that is taking 2 meals per day and most of the time Denise taking food.
Sleep was adequate
Bowel moments were regular
Addictions- patient used to smoke 2 packs per day stopped 5 years ago
Family history:-
No significant family history
General examination:-
Patient was drowsy(arousable) cooperative coherent
No pallor, icterus,cyanosis,lympadenopathy,edema of foot
Vitals on presentation
Temp:- 102F
Pr:- 148 bpm
Rr:- 44cpm
Bp:-80/50 mmHg
Spo2:- 88% on RA kept on 6litres of O2 then maintained 99%
GRBS:- high
On Respiratory system examination:-
On inspection:- normal shaped chest, trachea appears to be in centre, no scars and sinuses present,abdomino thoracic type of respiration, normal respiratory movements present
On palpation:- all inspectory findings are confirmed on palpation.
On percussion:- right left
Infraclavicular resonant resonant
Mammary dullnote. resonant
Axillary. resonant resonant
Infraaxillary. dullnote. resonant
Suprascapular. resonant. resonant
Infrascapular. dullnote resonant
Upper, mid, lower. resonant. resonant
Interscapular
On auscultation:- normal vesicular breath sounds heard and decreased breath sounds in right inframammary,infra axillary,infrasacpular areas.
On CVS examination:-normal JVP, S1,S2 present,no murmurs
Per abdomen:- soft and diffuse tenderness, central umbilicus.
CNS :
Right Handed person.
HIGHER MENTAL FUNCTIONS:
Conscious, oriented to time place and person.
speech : normal
Behavior : normal
Memory : Intact.
Intelligence : Normal
Lobar Functions :
No hallucinations or delusions.
MOTOR EXAMINATION:
Right Left
UL LL. UL LL
BULK Normal Normal Normal Normal
TONE Normal Normal Normal Normal
POWER 4/5, 4/5 4/5 , 4/5
SUPERFICIAL REFLEXES:
R. L
CORNEAL present present
CONJUNCTIVAL present present
ABDOMINAL present
DEEP TENDON REFLEXES:
R L
BICEPS 2+ 2+
TRICEPS 2+ 2+
SUPINATOR 2+ 2+
KNEE. 2+. 2+
ANKLE 2+. 2+
SPINOTHALAMIC SENSATION:
Crude touch
pain
temperature
DORSAL COLUMN SENSATION:
Fine touch
Vibration
Proprioception
CORTICAL SENSATION:
Two point discrimination
Tactile localisation.
steregnosis
graphasthesia.
PROVISIONAL DIAGNOSIS:- ?DKA
Investigations:-
CBP
Hb:-14
TLC:-13000
Platelet:-3.48
Hemogram
APTT:- 34sec
PT:- 17
INR:- 1.2
Blood grouping and Rh typing:-
Serology (HbsAg,HIV,HCV):-Negative
Urine for ketone bodies:- positive
Troponin-I :- 18.3
Repeat RFT on 3/12/23:-
Blood urea:-83
Serum creatinine:-2.2
Serum electrolytes
Na+ 148
K+ 3.8
Cl- 106
RFT on 2/12/23
Blood urea:- 111
Serum creatinine:- 2.3
Serum electrolytes
Na+ 145
K+ 4.2
Cl- 106
LFT:-
Direct bilirubin :- 1.63
Total bilirubin:- 0.24
SGOT:- 19
SGPT:- 15
Alkaline phosphate:- 229
Total proteins:- 6.3
Albumin: 2.97
A/g ratio:- 0.89
Cue
Sugars:- ++++
Albumin:- +
Pus cells:- 3-4 cells
Ketone bodies:- positive
Lipid profile
Total cholesterol:- 163mg/dl
Triglycerides:- 331mg/dl
HDL:- 38mg/dl
Ldl:- 88mg/dl
Vldl:-66.2mg/dl
HbA1C:- 7.5
FBS after 1 day of admission:- 70mg/dl
Rbs on admission:- 659mg/dl Rbs after 8 hours of insulin infusion:- 198mg/dl
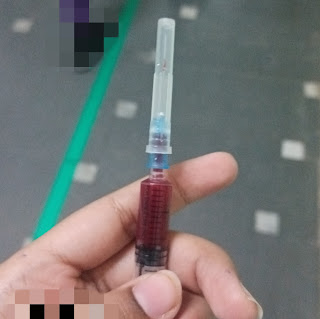
Serum potassium after 8 hours of insulin infusion:-
4.1mmol/L
Chest ray on presentation
Chest xray after admission
DIAGNOSIS:- Diabetic ketoacidosis with community acquired pneumonia with AKI (pre renal)
TREATMENT:-
Nbm till further orders
IV fluids NS @ 100ml/hr
Inj.piptaz 2.25mg IV TID
Inj.linezolid 600mg IV BD
Tab.azithromycin 500mg OD
Tab.Flucanazole 150mg OD
Inj.Human actrapid insulin @ 6 units/ hr
Tab.Metoprolol 25mg OD
Potassium infusion
20U-20U-20U-20U (6th hourly)
Inj.Pcm 1gm IV sos (if temp >101F)
Inj.lasix 20mg IV BD (if SBP >110 mmhg)
IV fluids- Frusidex @50 ml/hr
Tab.atorvas 40mg OD
Tab.clopitab-A 95/75 OD
Inj pan 40 mg IV OD
Right Handed person.
HIGHER MENTAL FUNCTIONS:
Conscious, oriented to time place and person.
speech : normal
Behavior : normal
Memory : Intact.
Intelligence : Normal
Lobar Functions :
No hallucinations or delusions.
MOTOR EXAMINATION:
Right. Left
UL. LL. . UL LL
BULK. Normal Normal Normal Normal
TONE. Normal Normal Normal Normal
POWER. 4/5, 4/5. 4/5 , 2/5
SUPERFICIAL REFLEXES:
R. . L
CORNEAL present. present
CONJUNCTIVAL present. present
DEEP TENDON REFLEXES:
R L
BICEPS 2+. 2+
TRICEPS 2+ 2+
SUPINATOR. 2+ 2+
KNEE. 2+. Couldn't be elicited
ANKLE - -
Plantar Flexor. Flexor
SPINOTHALAMIC SENSATION:
Crude touch. . +. +
pain. +. +
temperature. +. +
DORSAL COLUMN SENSATION:
Fine touch. . +. . +
Vibration. +. . +
Proprioception. +. +
CORTICAL SENSATION:
Two point discrimination +. . +
Tactile localisation. +. +
steregnosis. +. +
Checked for joint position at right metatarsophalangeal joint.







Comments
Post a Comment