My journey as an intern in department of General Medicine
I am Racha chandana , Intern posted in the General Medicine Department from 1/12/23 until 31/1/24.
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centred online learning portfolio and your valuable inputs on the comment box is welcome."I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
A 65 year old male patient with complaints of fever and sob
Complaints:-
Patient was brought to casualty with complaints of fever since one week
breathlessness since one day
history of presenting illness:-
Patient was apparently symptomatic one week back then he developed cough and cold which was insidious in onset associated with sputum, which was greenish in color and mucoid in nature,no aggravating factors no relieving factors then he developed the fever which was insidious onset , gradually progressive, it is of high grade, associated with chills and rigors for which he took medication from an RMP which got subsided but reappeared two days back
Patient complains of increased frequency of urine passage during night Times since 7 days( 4 to 5 times)
Complaints of decreased appetite since 4 days
Complaints of nausea since 4 days
Patient feels dehydrated Since 4 days complaints of dryness of lips
Complaints of shortness of breath since four days which was initially grade 2 which now progressed to grade 4 since last night.
Past history:-
No history of similar complaints in the past
complaints of pain in bilateral knee joints since 5 years for which he was using NSAID's
Not a known case of hypertension,TB, epilepsy,cva,CAD
Had a history of right tbl fracture 5 years back
Personal history:-
Patient takes normal diet, but due to decrease appetite he started to eat in less amount that is taking 2 meals per day and most of the time Denise taking food.
Sleep was adequate
Bowel moments were regular
Addictions- patient used to smoke 2 packs per day stopped 5 years ago
Family history:-
No significant family history
General examination:-
Patient was drowsy(arousable) cooperative coherent
No pallor, icterus,cyanosis,lympadenopathy,edema of foot
Vitals on presentation
Temp:- 102F
Pr:- 148 bpm
Rr:- 44cpm
Bp:-80/50 mmHg
Spo2:- 88% on RA kept on 6litres of O2 then maintained 99%
GRBS:- high
On Respiratory system examination:-
On inspection:- normal shaped chest, trachea appears to be in centre, no scars and sinuses present,abdomino thoracic type of respiration, normal respiratory movements present
On palpation:- all inspectory findings are confirmed on palpation
DIAGNOSIS:- Diabetic ketoacidosis with community acquired pneumonia with AKI (pre renal)
https://chandanaracharollno128.blogspot.com/2023/12/a-65-year-old-male-patient-with.html
Pajr link:-https://chat.whatsapp.com/H60z8QuyXwlB4LUacpoLCM
Case2:-
63 yr old male with fever and burning micturition since one month
Complaints:-
Complaints of increased frequency of passage of urine since one month
Vomiting Since one day
History of presenting illness
Patient was apparently a symptomatic one month back then he developed burning micturition which was insidious in onset, no aggravating and relieving factors
fever was insidious in onset, gradually progressive ,intermittent , associated with chills and rigors, low grade, relieved on medication
Complaints of vomiting since one day, non projectile, non bilious 4 episodes, food as content
Complaints of increased frequency of urine approximately 20 times a day and increased passage of urine during night Times approximately 5 times since 1 month
No history of cold and cough
Complaints of shortness of breath since 5 days
Patient feels Dehydrated since 5 days
No history of chest pain, palpitation ,syncope
Past history
History of RTA 1 year back, where he got admitted in the hospital used medication for diabetes, continued for 3 months, stopped by the patient as he felt alright after using the medication for 3 months,from then he has knee pains.
History of RTF 15 days back started to develop body pains since then
Uses NSAIDs daily to relieve the pain since 1 year
No history of similar complaints in the past
No history of hypertension,epilepsy , asthma, TB
Personal history
Patient works in a garage as a daily worker
He maintain normal diet
He sleep is adequate
Patient has constipation since 15 days, passes stools after 4 days, passes only after using medication
Bladder moments increased frequency of passage of urine since 1 month
Addictions consumes alcohol occasionally
Blog link:- https://chandanaracharollno128.blogspot.com/2023/12/a-63-yr-old-male-with-fever-and-burning.html
PaJr link:- https://chat.whatsapp.com/H60z8QuyXwlB4LUacpoLCM
Case 3:-
67 year old male with sob since 10 days,pedal and facial edema since 8 days
A 67 year old Male R/O Devarakonda , came to the casualty on 2nd December 2023 with complaints of Shortness of breath since 10 days and pedal & facial edema since 8 days
HISTORY OF PRESENT ILLNESS:
Patient came in drowsy but arousable state to the casualty . He was apparently asymptomatic 10 days back , then he developed Shortness of breath which is insidious in onset, gradually progressive in nature, aggravating on exertion and relieved on taking rest, progressed from grade II to grade III- IV (Modified MRC)
Orthopnea, Paroxysmal nocturnal dyspnea present
C/O Bilateral pedal edema below knees , facial puffiness and periorbital edema since 8 days , insidious onset, gradually progressive in nature , no diurnal variation, pitting type I.
C/o decreased urine output and decreased appetite since 5days
No C/o chest pain, palpitations, profuse sweating,
No c/o fever, cold, cough, nausea, vomiting, loose stools.
His daily routine is waking up at 6: 00 am, breakfast as idli/upma at 8:00 am . He used to have his lunch as rice and curry , sambhar/rasam at 1: 00 pm .He usually haves his dinner as chapati/upma/rice and curry at 8:00pm and goes to bed by 9:00 pm.
The patient used to lead a normal life before this 15days .
HISTORY OF PAST ILLNESS:
K/c/o asthma since 10yrs -on medication
N/K/C/O DM, CAD, CVD, Thyroid, epilepsy
K/C/O HTN 6 yrs ago and used medication for 3 yrs and stopped as BP was under control
H/O TB 30 yrs ago
PERSONAL HISTORY:
Married
Shop keeper by occupation
Diet: Mixed
Appetite: decreased
Sleep: adequate
Urine output decreased
Bowel movements: Regular
Addictions: Alcohol occasionally
Allergies: no known
GENERAL EXAMINATION:
Patient is drowsy due to sedation, coherent to time , place, person.
Ht: 155cm Wt: 58 kg
Pallor: present
Icterus: absent
Clubbing: absent
Cyanosis: absent
Koilonychia: absent
Lymphadenopathy: absent
Post intubation vitals: Vitals: Temp: 98 F
BP: 90/60 mmHg
PR: 102 bpm
RR: 15 cpm ACMV mode
SpO2: 100% at 5 litre O2
GRBS: 126 mg%
SYSTEMIC EXAMINATION:
RS:
Orthopnea +
Paroxysmal nocturnal dyspnoea +
wheeze +
Central position of trachea
NVBS +
CVS:
S1 S2 heard
No murmurs
No thrills
ABDOMEN:
Shape of abdomen: mildly distended
No tenderness
No palpable mass
No bruits
Liver and spleen- not palpable
Bowel sounds heard
CNS:
drowsy but arousable
no neck stiffness
kernig's sign negative
cranial nerves: normal
motor - intact
sensory - intact
Glasgow scale E2V2M2 = 6/15
MUSCULOSKELETAL SYSTEM: normal
SKIN: normal
ENT: normal
TOOTH & ORAL CAVITY: normal
Provisional diagnosis:- ?Acute kidney injury
Blog link:-
https://chandanaracharollno128.blogspot.com/2023/12/a-67-year-old-male-ro-devarakonda-came.html
Case 4:-
55 year old with generalised body swelling since 15 days
Complaints:-
C/o generalised body swelling since 15 days
C/o shortness of breath since 10 days
C/o decreased urine output since 10 days
C/o fever since 2 days
History of presenting illness:-
Patient was apparently asymptomatic 15 days back then noticed generalised body swelling (Anasarca) since then
C/0 shortness of breath since 10 days, insidious in onset, gradually progressive, from grade I to grade III, orthopnea present, No PND
C/o decreased urine output since 10 days, burning micturition present,
No C/o cough, nausea, vomiting , loose stools
Past history:-
K/C/O DM since 6 years and is on inj.Human Actripid Insulin 10U--10U--10U
K/C/O HTN since 1 year and is on Tab.amlodipine 10mg OD
k/c/o CKD since 1 year and is on conservative management.
N/K/C/O CAD, CVD, Thyroid disorders, epilepsy
Personal history:-
Diet :-
Addictions:- stopped smoking 5 years ago.
Used to smoke beedi 2 packs/day
Used to drink alcohol occasionally,stopped drinking 5 years ago
Sleep:- adequate
Bowel and bladder movements:- decreased urine output since 10 days,bowel movements regular
Patient is drowsy due to sedation, coherent to time , place, person.
Pallor: present
Icterus: present
Clubbing: absent
Cyanosis: absent
Lymphadenopathy: absent
PR: 102 bpm
RR: 15 cpm
SpO2: 100% at 5 litre O2
GRBS: 126 mg%
Provisional diagnosis:- ??CKD secondary to diabetes
Blog link:- https://chandanaracharollno128.blogspot.com/2023/12/is-online-e-log-book-to-discuss-our.html
OP DUTY;-
i have seen multitude of cases in the op,there was an interesting day among them where i have seen many chest pain cases over 10 ,only one among them was diagnosed to have inferior wall MI (he was in a window period).
he was a 42 year old male presented to general medicine opd at 10am
with complaints of severe burning type of chest pain since 8am, substernal radiating to left arm was not relieved on medication.serial ecgs done which showed ST elevation in lead II,III and aVF.
2d echo showed ef:-55%, good contraction of Left ventricle.
Serial ecgs
2d echo
Posted in psychiatry:-
These are the cases which i have seen while i was in psychiatry
learning points which i have learnt while I was posted in psychiatry:-
how to interact with a patient with patience,to diagnose the condition just by listening to their story which brought them here and one cannot get into conclusion without informants view of story.
Posted in peripherals
I faced many challenges while i was posted in ICU
One such challenge was to revive a patient(which was a case of decompensated liver cirrhosis) whose saturations were dropping rapidly with sp02 being 60% ,heart rate being 170 ,respiratory rate 50cpm
immediately started doing cpr , patient was not revived , vitals were still unstable ,they i assisted in doing intubation(did ambu), patient was not still revived ,ecg flat line achieved.Unfortunately patient couldnt be revived.
learning points
learnt how to perform a quality CPR
how to insert a ryles tube
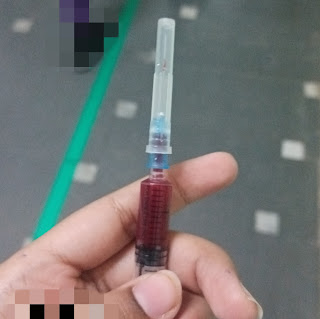
how to take an ABG sample
how to monitor the patients
Nephrology :-
learning points:-
learnt how the dialysis machine works, how it helps the patients who landed in chronic renal failure.
how to monitor the patients who are undergoing dialysis
performed 5 blood transfusions
collected 5 ABG samples















Comments
Post a Comment