67 year old male with sob since 10 days,pedal and facial edema since 8 days
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment.
A 67 year old Male R/O Devarakonda , came to the casualty on 2nd December 2023 with complaints of Shortness of breath since 10 days and pedal & facial edema since 8 days
HISTORY OF PRESENT ILLNESS:
Patient came in drowsy but arousable state to the casualty . He was apparently asymptomatic 10 days back , then he developed Shortness of breath which is insidious in onset, gradually progressive in nature, aggravating on exertion and relieved on taking rest, progressed from grade II to grade III- IV (Modified MRC)
Orthopnea, Paroxysmal nocturnal dyspnea present
C/O Bilateral pedal edema below knees , facial puffiness and periorbital edema since 8 days , insidious onset, gradually progressive in nature , no diurnal variation, pitting type I.
C/o decreased urine output and decreased appetite since 5days
No C/o chest pain, palpitations, profuse sweating,
No c/o fever, cold, cough, nausea, vomiting, loose stools.
His daily routine is waking up at 6: 00 am, breakfast as idli/upma at 8:00 am . He used to have his lunch as rice and curry , sambhar/rasam at 1: 00 pm .He usually haves his dinner as chapati/upma/rice and curry at 8:00pm and goes to bed by 9:00 pm.
The patient used to lead a normal life before this 15days .
HISTORY OF PAST ILLNESS:
K/c/o asthma since 10yrs -on medication
N/K/C/O DM, CAD, CVD, Thyroid, epilepsy
K/C/O HTN 6 yrs ago and used medication for 3 yrs and stopped as BP was under control
H/O TB 30 yrs ago
FAMILY HISTORY:
Not significant
PERSONAL HISTORY:
Married
Shop keeper by occupation
Diet: Mixed
Appetite: decreased
Sleep: adequate
Urine output decreased
Bowel movements: Regular
Addictions: Alcohol occasionally
Allergies: no known
GENERAL EXAMINATION:
Patient is drowsy due to sedation, coherent to time , place, person.
Ht: 155cm Wt: 58 kg
Pallor: present
Icterus: absent
Clubbing: absent
Cyanosis: absent
Koilonychia: absent
Lymphadenopathy: absent
Post intubation vitals: Vitals: Temp: 98 F
BP: 90/60 mmHg
PR: 102 bpm
RR: 15 cpm ACMV mode
SpO2: 100% at 5 litre O2
GRBS: 126 mg%
SYSTEMIC EXAMINATION:
RS:
Orthopnea +
Paroxysmal nocturnal dyspnoea +
wheeze +
Central position of trachea
NVBS +
CVS:
S1 S2 heard
No murmurs
No thrills
ABDOMEN:
Shape of abdomen: mildly distended
No tenderness
No palpable mass
No bruits
Liver and spleen- not palpable
Bowel sounds heard
CNS:
drowsy but arousable
no neck stiffness
kernig's sign negative
cranial nerves: normal
motor - intact
sensory - intact
Glasgow scale E2V2M2 = 6/15
MUSCULOSKELETAL SYSTEM: normal
SKIN: normal
ENT: normal
TOOTH & ORAL CAVITY: normal
PHYSICAL EXAMINATION:
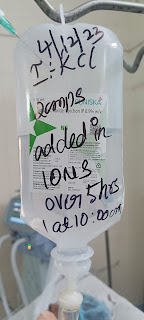
IVF NS 100ml IV 100ml/hr
Inj.noradrenalin @2mcg/min to maintain MAP >65mmhg
Inj.midazolam 2400mcg/hr
Ryles feeds 50 ml 2nd hourly
Inj.piptaz 2.25 gm IV TID
Inj.linezolid 600mg IV BD
Et tube suction 2nd hourly
Chest physiotherapy
Patient vitals remained same until 7/12/23
Midazolam IV stopped to try to extubate the patient,patient didn't regain the consciousness and passed away after few days even after performing quality CPR and giving the all necessary drugs







Comments
Post a Comment