55 year old with generalised body swelling since 15 days
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment.
Complaints:-
C/o generalised body swelling since 15 days
C/o shortness of breath since 10 days
C/o decreased urine output since 10 days
C/o fever since 2 days
History of presenting illness:-
Patient was apparently asymptomatic 15 days back then noticed generalised body swelling (Anasarca) since then
C/0 shortness of breath since 10 days, insidious in onset, gradually progressive, from grade I to grade III, orthopnea present, No PND
C/o decreased urine output since 10 days, burning micturition present,
No C/o cough, nausea, vomiting , loose stools
Past history:-
K/C/O DM since 6 years and is on inj.Human Actripid Insulin 10U--10U--10U
K/C/O HTN since 1 year and is on Tab.amlodipine 10mg OD
k/c/o CKD since 1 year and is on conservative management.
N/K/C/O CAD, CVD, Thyroid disorders, epilepsy
Personal history:-
Diet :-
Addictions:- stopped smoking 5 years ago.
Used to smoke beedi 2 packs/day
Used to drink alcohol occasionally,stopped drinking 5 years ago
Sleep:- adequate
Bowel and bladder movements:- decreased urine output since 10 days,bowel movements regular
Family history:- not significant
GENERAL EXAMINATION:
Patient is drowsy due to sedation, coherent to time , place, person.
Pallor: present
Icterus: present
Clubbing: absent
Cyanosis: absent
Lymphadenopathy: absent
PR: 102 bpm
RR: 15 cpm
SpO2: 100% at 5 litre O2
GRBS: 126 mg%
SYSTEMIC EXAMINATION:
RS:
Orthopnea +
Paroxysmal nocturnal dyspnoea +
wheeze +
Central position of trachea
NVBS +
CVS:
S1 S2 heard
No murmurs
No thrills
ABDOMEN:
Shape of abdomen: mildly distended
No tenderness
No palpable mass
No bruits
Liver and spleen- not palpable
Bowel sounds heard
CNS: no focal neurological deficits
Provisional diagnosis:- ??CKD secondary to diabetes
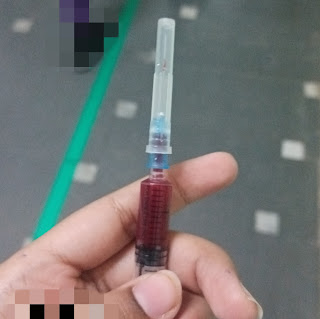
Investigations:-
Urea:-87
Creatinine:-6.4
K+:-3.1
Hb:-7.7
TLC:-11099
N/L/E/m:-82/12/0/6
6 hemodialysis were done to this patient
Post dialysis serum urea level was 10mg/dl
Serum creatinine:- 3.8 mg/dl
K+:-3.7 mEq/L
Diagnosis -chronic kidney disease secondary to diabetes(diabetic nephropathy)
Anemia of chronic disease ( secondary to CKD)
Type2 respiratory failure
Treatment:-
Inj.ceftriaxone 1gm IV/BD for 5 days
Inj.piptaz 4gm IV stat followed by 2.25 gm IV TID for 4 days
Inj.clindamycin 600mg IV BD for 4 days
Inj.lasix 50mg IV BD
Inj HAI according to GRBS
Inj.EPO 5000units s/c weekly once
Tab.amlodipibne 5mg po OD
Tab nodosis 500 mg po BD
Intermittent Bipap
Tab.shelcal po OD








Comments
Post a Comment