A 42 year old male with body pains and fever
This is an E log book to discuss our patient's de-identified health data shared after taking his guardian's signed informed consent. Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable comments in comment box are most welcomed
I have been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency i reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan
Chandana racha
Roll no 128
Chief complaints:- fever since 6 days
vomitings on and off since 4 days
Shortness of breath since 2 days
Yellowish discoloration of urine since 1 day
A 42 year old male, farmer by occupation, came to the OPD 9 days ago with complaints of fever, body pains, yellowish discoloration of the eyes and vomiting since the previous day.
The patient was apparently asymptomatic 17 days ago. He then had decreased appetite for a week before he developed fever, body pains, yellowish discolouration of sclera and vomitings. He then got admitted to this hospital.
HISTORY OF PRESENT ILLNESS:-
The patient has had a habit of drinking alcohol around 3 times a week since many years.
2 years ago, the patient's wife passed away, which increased the amount of drinking.
17 days ago, the patient started having a decreased appetite because of his drinking habits.
10 days ago, the patient went to work to spray pesticides in the field as a part of his work. In the evening, the patient drank 90ml of alcohol and lost his appetite completely, associated with fullness of abdomen. He felt body pains and was found to have a fever,which was intermittent with medication. He also vomited. The vomit consisted of dal from his lunch. He didn't eat anything else that night.
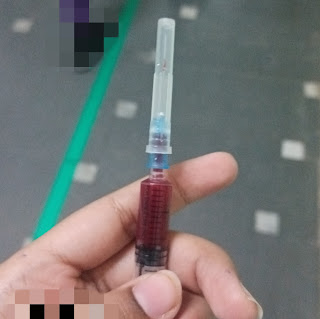
The next day (9 days ago), he was taken to an RMP, who took his blood sample. It was found that his blood cell counts were low. He was then taken to another government hospital, where the doctors told him that his liver was damaged by his alcohol consumption. He was also told his kidney is not actively functioning and need for dialysis and then given glucose and referred to this hospital. He had hypochondrial pain with tenderness. He also had pruritus and fullness in his abdomen.
2-3 days after admission (7 days ago), the patient developed generalised swelling all over the body with body pains and tenderness in the hypochondrial region. He also didn't eat anything for these 2-3 days and was on fluids.
3 days ago, the patient's swelling and body pains got relieved with the medication, including the hypochondrial pain.
He underwent dialysis for 3 times in a week
There is no history of burning Micturition, loose stools. No history of cough, itching, rashes
.HISTORY OF PAST ILLNESS:-
No similar complaints in the past.Not a known case of diabetes, hypertension, CAD, CVA, asthma, tuberculosis, epilepsy. History of rodent exposure.
Treatment history:- not significant
PERSONAL HISTORY:-
Diet: mixed
Appetite: decreased
Bowel movement: regular
Micturition: normal but yellowish discoloration since 1 day.
Addictions: alcohol consumption around 3 times a week since many years
FAMILY HISTORY:-
Not significant
PHYSICAL EXAMINATION:-
General examination:-patient is examined in supine position with his consent in well illuminated area.
(At the time of admission)
The patient is conscious, coherent and cooperative.
He is well built and moderately nourished.
Pallor - absent
Icterus - presentNo clubbing, cyanosis, lymphadenopathy, pedal edema
Patient is mildly dehydrated
Pedal edema was present on admission
Vitals:-
Temperature: 99 F
Pulse rate:100 bpm
Respiratory rate: 22 breaths/min
Blood pressure: 110/80mmHg
SPO2: 97%
GRBS: 126mg%
SYSTEMIC EXAMINATION:-
Abdomen:-
Inspection:- shape of abdomen:- distended.All quadrants move with respiration, umbilicus is inverted, no engorged veins, no visible pulsations, no scars and sinuses present.
Palpation:- no local rise of temperature, localized pain over right Hypochondrium,shifting dullness was present. Kidneys are ballotable.
Percussion :-
CNS:-
The patient was conscious, coherent cooperative and .







Comments
Post a Comment