1801006137-SHORT CASE
I have been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency i reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan
Chandana racha
1801006137
Presentation
https://youtu.be/QsYhokW3L2g
https://youtu.be/HWKa0PSta7U
A 20 yr old girl came to casualty with chief complaints of
Pedal edema since 15 days
Hyperpigmented macules since 15days
Fever since 15 days
cough(dry)since 7 days
decreased appetite since 7 days
shortness of breath since 5 days
decreased urine output since 3 days
Abdominal distension since 1 day
lost ability to speak since 1 day
HOPI:-
Patient was apparently asymptomatic 15 days back then she developed bilateral pedal edema extending till knees which was insidious in onset, gradually progressive no aggravating and relieving factors , for which she took some medication for which she complained of developing hyperpigmented macules on her face then she stopped taking medication.
After 2 days of stopping medication she again complained of developing bilateral pedal edema
Along with pedal edema she developed fever which was high grade continous in nature associated with chills since 5 days with no history of evening rise of temperature, no headache, no sweating.
Then she developed abdominal distension 8 days back which was insidious in onset, gradually progressed to present size.
Then she developed cough, which was insidious in onset, non productive.relieved on medication??
Then she developed decreased appetite one week back.
Then 5 days back she developed shortness of breath,insidious in onset, progressive in nature, to which she got admitted in other hospital and then she was referred to this hospital. She also had history of constipation and decreased urine output since 3 days.
then one day back she developed aphasia which was sudden in onset ,for which she was admitted in government hospital nalgonda ,but later shifted to our hospital.
Past history:- no similar complaints in the past and not a known case of diabetes mellitus, hypertension, asthma, thyroid, coronary artery disease, epilepsy, TB
Personal history:-
Mixed diet
Appetite lost
Non veg diet
Decreased bowel and bladder movements
Family history:- no significant family history
On Examination:-
Patient was Conscious, coherent, non cooperative well oriented to time, place and person. On admission vitals are.
RR 24cpm
Bp 110/70
PR 112bpm
Sp02 97%
Temp 99.8
On Respiratory system examination:-
On inspection:- normal shaped chest, trachea appears to be in centre, no scars and sinuses present,abdomino thoracic type of respiration, normal respiratory movements present
On palpation:- all inspectory findings are confirmed on palpation.
On percussion:- right left
Kornigs isthmus
Infraclavicular
Mammary
Axillary
Infraaxillary
Suprascapular
Infrascapular
Upper, mid, lower
Interscapular
On auscultation:- normal vesicular breath sounds heard with inspiratory wheeze heard in all areas and left infrascapular crepts present
On CVS examination:-raised JVP, apex placed laterally, palpable thrill in Mitral area, loud S2 heard , pansystolic murmur in mitral area
Per abdomen:- soft and nontender, central umbilicus.
On CNS examination:- bilateral upper limb hypertonia with exaggerated deep tendon reflexes
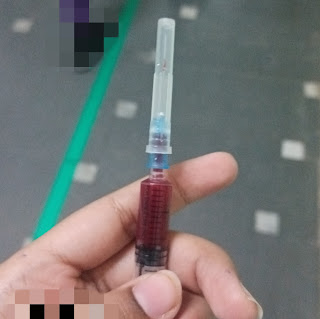
CNS :


























.jpg)














Comments
Post a Comment